by Nathan Villasenor, Natalee Gonzalez, and Olivia Williams
The communication scholar our group chose to interview was Jasmine Phillips. She has a PhD in communications and is a professor here at Cal State Fullerton. The published study we decided to interview Dr. Phillips on was “A Community-Based Approach to HIV Prevention: Engaging Mayan Young Adults in Rural Guatemala“. Dr. Phillips and her team conducted their research in Santiago Atitlán, which is located in the Sololá state of Guatemala. They were inspired to do their research specifically on the Mayan people in Guatemala because they represent 40% of the country’s population and account for 20% of their HIV cases. An interesting point of this study was that, even though the rates of HIV within the Guatemalan community were growing, they were still very low. This led the research team to work backwards to justify the use of the population. The Mayan people have a lack of HIV knowledge and extremely limited access to medical treatment, making them vulnerable to a potential outbreak. The research aimed to raise awareness about HIV within their community.
Dr. Phillips was inspired to join this study due to her interest in public health, health campaigns, and intercultural/international research. A part of the interest in this study is because it aims to change people’s behaviors. This study is a perfect combination. The study aims to learn about a foreign population’s knowledge of HIV, to further educate them on the prevention of HIV in hopes that they change the communities perception on HIV and help them learn and practice preventative measures.
Dr. Phillips and her team decided they wanted to do both a qualitative and quantitative study. They decided to break up their research into two phases. Both phases included the approach of community-based participatory research or CBPR. The CBPR approach invloves close cooperation with researchers and the target audience to create knowledge about HIV in the community to improve health outcomes. The team wanted to take the CBPR approach because the study was rooted in community collaboration, and CBPR allows for the team to work directly with the community and receive input on how the research was designed. Dr. Phillips was asked why the team wanted to take a qualitative and quantitative method and not juts do mass surveys. She responded by saying they wanted to take the CBPR approach because they did not want to follow the typical international research route. Dr. Phillips said, typically the U.S researchers go to other countries and assume the communities needs due to viewing themselves as the experts. Going in with this approach ends with failure due to not understanding the culture, communication styles, and lacking knowledge about the population.
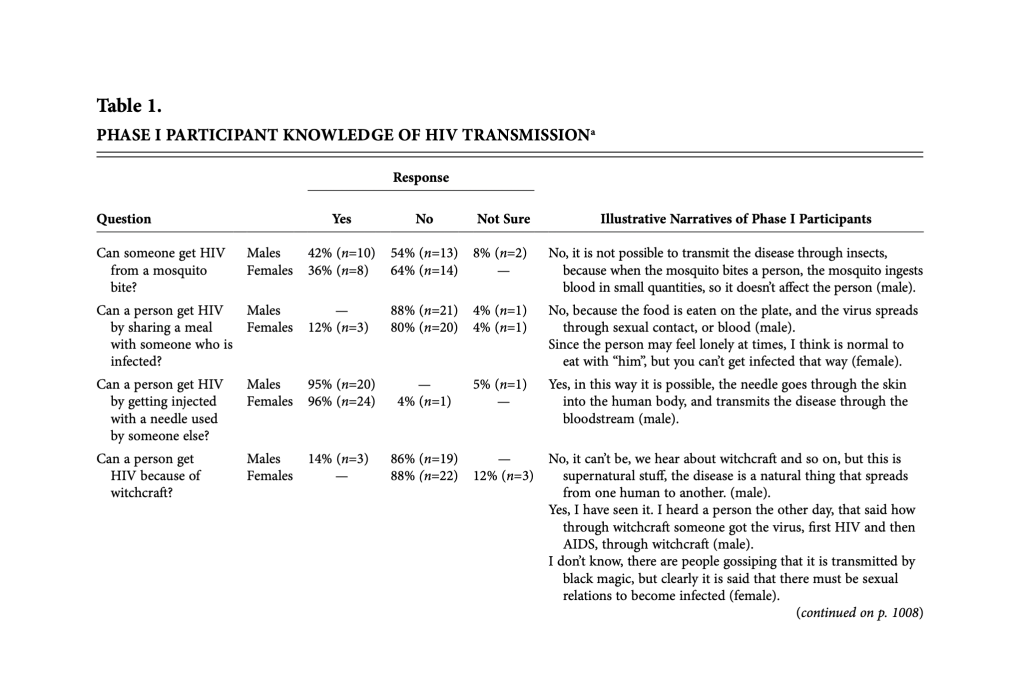
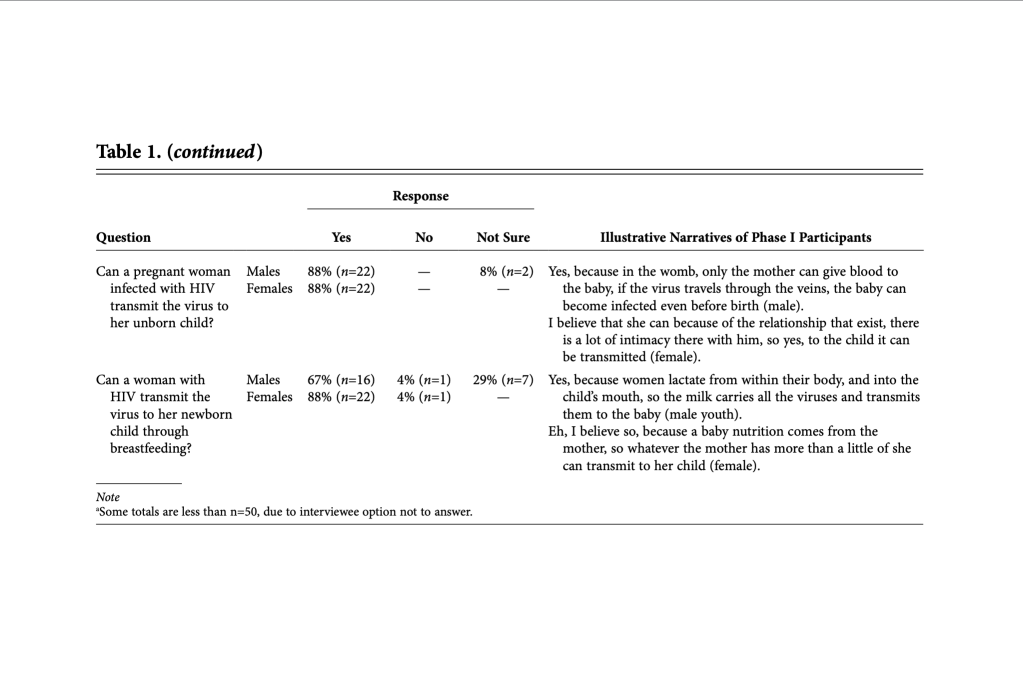
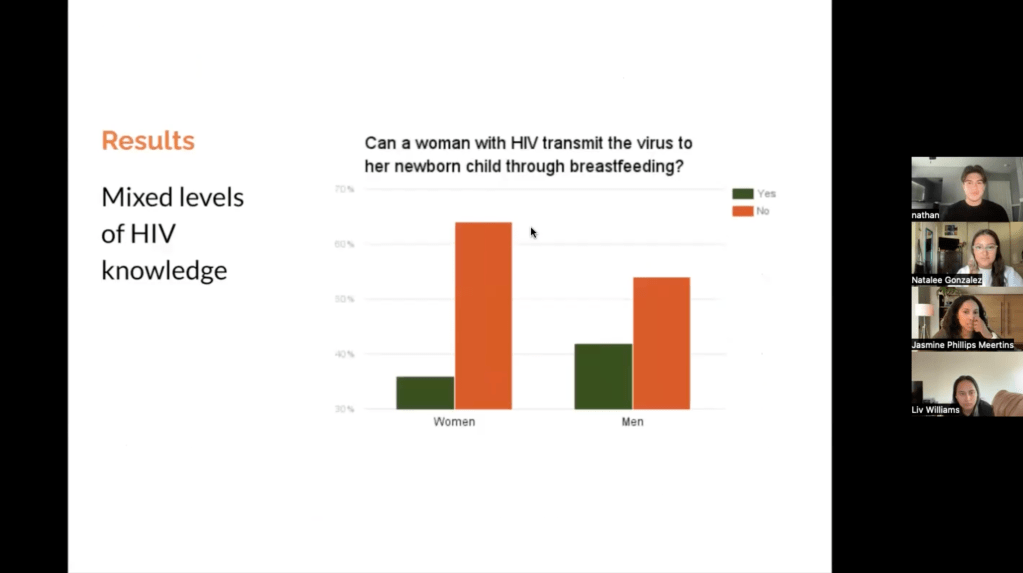
The CBPR approach requires a volunteer sample. They were successful in getting volunteers by collaborating with the government, local coordinators, and local educators. They reached out to the community via radio announcements and posted flyers around town to inform them about the study. Dr. Phillips mentions the usage of radio announcements and flyers were the best way to communicate with locals because there weren’t many TVs, phones, or Wi-Fi. Phase one applies the quantitative study method by giving the participants a survey about HIV adapted from the Center for Disease Control and Prevention (CDC). The survey used a likert scale with the options of yes, no, not sure, depends.
With the decision to approach the study using CBPR, the team had to decide on the most efficient way to bring volunteers to speak about a topic that was seen as taboo. Reflecting back on the team’s choice to bring attention to the study through radio announcements and flyer distribution, Dr. Phillips spoke about what she would do differently now. Dr. Phillips believes that determining the most effective way to attract volunteers comes down to what your population looks like. Because their population was based out of a small community, aside from the radio and flyers, word of mouth is the best way to recruit volunteers to participate in the study. Since the study was done in a different country, the team was not there from start to finish; instead, they made visits. Looking back, Dr. Phillips believes that having a researcher on location the whole time could have proven more effective in order to build trust with the community and get more honest answers.
The sample for this study consisted of only heterosexual adult participants living in the rural Tz’utujil Mayan town of Santiago. When asked about how Dr. Phillips believed the results of the study would have changed if the sample were to open up the limitations on sexual orientation, as well as having the age limit lowered, Dr. Phillips provided a simple answer. To conduct this study on the LGBTQ+ community within Tz’utujil, they would have to conduct a completely new study with a focus on this group because the needs of this population can differ vastly from that of heterosexuals. As well with the age limit, there are practical barriers that the team would have to work through in order to protect minor participants. With these barriers in place to protect the minor participants, an example being having their parents sit in and listen to their answers, it could have a major impact on the answers which could lead to faulty conclusions. Although due to these limitations, it opens up the door for other researchers to conduct this study on these unrepresented communities.
One of the key takeaways from Dr. Phillips research was that the culture plays a key role in understanding. In this case, the Mayan people’s perception of HIV was influenced by their community, their history, and their experiences. The ultimate goal of the research was to inform and abolish those old beliefs the Mayan people had of HIV, as well as to do away with any misinformation they may have, According to Dr. Phillips, HBM (Health Brief Model) was useful in identifying young Mayan adults’ susceptibility to HIV. Another method of research that was used during the study was the likert scales. This allowed for questions to be answered based on how they felt, ranging from agree, neutral, and disagree. As effective as it was, the design had its flaws and limitations. A problem Dr. Phillips ran into during the study was the worry of asking questions that were too personal, in fear of making the participants uncomfortable since sex was seen as a taboo topic. To overcome this, during the second phase of the research study, Dr. Phillips had talked to the leaders of the Mayan community to conduct the interviews themselves in order for those who were being interviewed to feel more comfortable. With this method, talking about HIV and sex felt less inappropriate. Despite the bumps in the road, the findings of the research were still able to successfully conduct a tailored HIV prevention campaign plan. Dr. Philips said herself that her goal was to help international, undeserved populations abroad. She also said that through this research they recognize the influenxe of culture and engagement to improve community health promotion, which is the most important fact.